4 min read
Electromyography (EMG)
Electromyography (EMG) is a technique that captures and analyzes the electrical activity produced by skeletal muscles. The roots of EMG trace back to the early studies of muscle and nerve physiology in the 19th century. Luigi Galvani, in the 18th century, had already conducted experiments demonstrating that frog muscles produced electricity. However, it wasn’t until the invention of the electroencephalogram (EEG) in the 1920s that scientists began to deeply explore the possibility of recording muscle electrical activity. Advancements in amplification technology during the 20th century led to the development of EMG devices that could precisely record muscular activity. Over time, EMG has solidified its role as an indispensable tool in clinical neurology, rehabilitation, and biomechanics research.

Basic principles of electromyography
Electromyography operates on the principle that when a muscle contracts, it generates electrical impulses. These impulses, or action potentials, are produced by the depolarization of muscle fibers in response to nerve signals. By placing electrodes on the skin or directly inserting them into the muscle, it becomes possible to record this electrical activity. The obtained recordings, termed electromyographic tracings, represent the summation of all action potentials from muscle fibers near the electrodes. By analyzing these tracings, physicians and scientists can determine whether a muscle is functioning normally or if it displays any anomalies. Furthermore, through studying the shape, duration, amplitude, and frequency of the recorded potentials, detailed information can be gleaned regarding the integrity and functionality of both muscles and the nerves innervating them.
Procedure: Preparation, electrode placement, and data acquisition
1. Preparation: Before starting an EMG test, it’s crucial to ensure the patient is comfortable and informed about the procedure. The skin must be cleaned to remove any oils, sweat, or lotions, which can interfere with the quality of the recorded signals. It’s also important to ensure the patient is relaxed since muscle tension can affect the readings. Any electronic devices or jewelry in the vicinity should be removed to prevent interference.
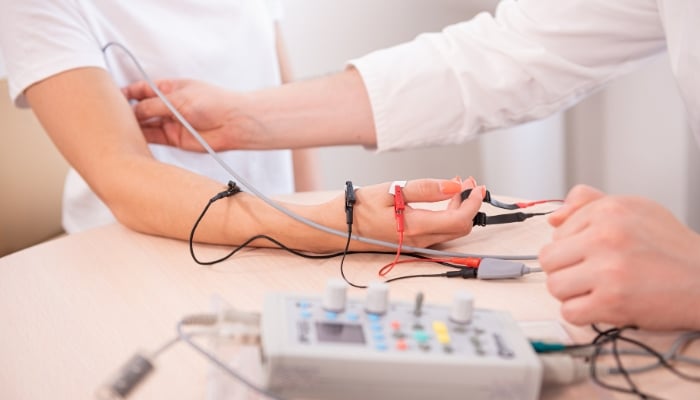
2. Electrode Placement: There are two primary types of electrodes used in EMG: surface electrodes and needle electrodes. Surface electrodes are adhesive pads that are placed on the skin over the muscle being studied. They are typically used for recording superficial muscle activity. In contrast, needle electrodes are thin, fine needles inserted directly into the muscle tissue. Their placement requires precise knowledge of the muscle anatomy and the specific areas of interest. The choice of electrode depends on the nature of the study, the depth of the muscle being examined, and the clinical questions being addressed.
3. Data Acquisition: Once the electrodes are correctly placed, the patient may be asked to contract the muscle gently. The electrical activity produced during this contraction is then picked up by the electrodes, amplified by the EMG machine, and displayed as waveforms on a monitor. The healthcare professional will observe these waveforms, listening to the sounds made by the electrical discharges. This activity may be recorded at rest, during voluntary contraction, and during the muscle’s passive stretch. Different muscles and conditions will produce distinct patterns on the EMG, and interpreting these patterns requires skill and experience. The entire procedure can last anywhere from 30 minutes to an hour, depending on the number of muscles being tested and the specific details of the examination.
Types of EMG
1. Surface EMG
Surface Electromyography (sEMG) is a non-invasive procedure that uses electrodes placed on the skin’s surface to measure the electrical activity of the underlying muscles. Unlike needle EMG, where electrodes penetrate the skin, sEMG is entirely external. This makes sEMG especially useful for patients who may be apprehensive about needles or when monitoring large muscle groups.
Advantages:
- Non-invasive and painless
- Can record from multiple muscle groups simultaneously
- Ideal for dynamic studies, such as gait analysis.
Limitations:
- Can’t detect the activity of deep muscles.
- More susceptible to interference, such as from nearby electrical devices.
Applications: Commonly used in sports medicine to study muscle function, physical therapy to monitor rehabilitation progress, and biomechanics research.
2. Intramuscular EMG
Intramuscular EMG, often simply called «needle EMG», involves inserting a thin needle electrode directly into the muscle tissue. This allows for a more detailed and localized measurement of muscle activity. The needle acts both as a recording and referencing electrode, picking up electrical signals from the muscle fibers closest to it.
Advantages:
- Provides a detailed analysis of individual muscle fibers
- Can study deep muscles not accessible with surface EMG
- Less affected by external interference.
Limitations:
- Invasive procedure that can be uncomfortable for the patient
- Measures a smaller area, so might miss overall muscle activity
Applications: Widely used in clinical settings to diagnose neuromuscular disorders, evaluate nerve damage, or determine the source of unexplained muscle weakness.

Clinical Applications and Diagnoses
1. Neuromuscular disorders: Electromyography plays a critical role in diagnosing various neuromuscular disorders. When nerves or muscles are damaged, the electrical activity changes, and these changes can be detected using EMG. Common neuromuscular conditions diagnosed or evaluated with EMG include:
- Myopathies: These are muscle disorders where the primary defect lies within the muscle tissue itself. EMG can detect abnormal spontaneous activity, indicating muscle fiber damage or inflammation.
- Neuropathies: Diseases that affect the peripheral nerves. An EMG can help determine whether the nerve damage is due to axonal degeneration or demyelination
- Motor neuron diseases: Such as amyotrophic lateral sclerosis (ALS). EMG can detect the widespread denervation indicative of these conditions.
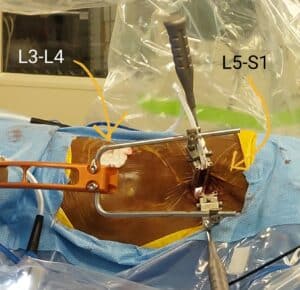
2. Spinal cord injuries: For patients who have suffered spinal cord injuries, EMG can help ascertain the severity and level of the injury. It’s especially valuable in cases where imaging studies are inconclusive. By evaluating the muscle activity below the injury level, clinicians can better predict the potential for recovery and plan appropriate rehabilitation strategies.
3. Muscle inflammation and injuries: In instances of muscle trauma, inflammation, or other localized injuries, an EMG can help pinpoint the affected muscle regions and the injury’s nature. This is particularly useful in sports medicine, where accurate diagnosis is vital for effective treatment and preventing long-term damage.
4. Evaluating the effectiveness of treatments: After initiating treatments for neuromuscular conditions or injuries, EMG can serve as a monitoring tool. By comparing the electrical activity of muscles before and after treatments, clinicians can evaluate the treatment’s effectiveness and make necessary adjustments.
Limitations of EMG
Despite its value in neurology and medicine, EMG has its limitations:
- Surface vs. Intramuscular recordings: While surface EMG is non-invasive, it can’t measure deep muscle activity as effectively as intramuscular EMG. Conversely, intramuscular EMG, being invasive, might not be suitable for all patients or scenarios.
- Interference: Both types of EMG can be affected by external factors, such as electrical equipment in the vicinity or even the patient’s body temperature.
- Skill and interpretation: The results of an EMG test largely depend on the skill of the person performing the test and interpreting the results. Misinterpretations can lead to inaccurate diagnoses.
- Doesn’t provide a complete picture: While EMG can detect abnormalities in muscle and nerve function, it may not always pinpoint the exact cause of a disorder. Other tests or clinical evaluations might be necessary.
Recent Advances and Future Directions
1. Technological improvements in electrode design: En los últimos años, hemos visto avances significativos en el diseño de electrodos utilizados en EMG. Estos nuevos diseños buscan mejorar la precisión de las lecturas, minimizar el malestar del paciente y permitir una mejor adaptabilidad a diferentes situaciones clínicas. Por ejemplo, se están desarrollando electrodos más pequeños, flexibles y biocompatibles, que pueden permanecer en el cuerpo durante períodos más prolongados sin causar irritación. Además, la mejora en la calidad del material utilizado en los electrodos ha permitido una captura de señal más clara y menos susceptible a interferencias externas.
2. Integration with other diagnostic modalities: La integración de EMG con otras modalidades diagnósticas está abriendo nuevas fronteras en el campo de la neurología y la medicina del deporte. Un ejemplo prominente es la combinación de EMG con técnicas de imagen, como la resonancia magnética (MRI) o la ecografía. Esta combinación permite a los médicos visualizar la estructura muscular y los nervios al mismo tiempo que evalúan su función, proporcionando un panorama más completo del estado del tejido neuromuscular del paciente. Tal integración promete no solo mejorar la precisión diagnóstica sino también guiar tratamientos y procedimientos intervencionistas con mayor precisión.
3. New applications in rehabilitation and therapy: El EMG no solo es una herramienta diagnóstica, sino que también está encontrando nuevas aplicaciones en el campo de la rehabilitación y la terapia. Con la capacidad de monitorizar la actividad muscular en tiempo real, los terapeutas pueden obtener retroalimentación instantánea sobre el rendimiento muscular de un paciente. Esto es particularmente útil en pacientes que se recuperan de lesiones, permitiendo ajustes en tiempo real en su régimen de rehabilitación. Además, los sistemas EMG están siendo integrados en dispositivos de asistencia robótica, lo que permite a los pacientes que han sufrido daño neuromuscular controlar prótesis o exoesqueletos con sus señales musculares.